The pace of new hospitalizations for COVID-19 is increasing so rapidly in Los Angeles County that it is now literally off the charts, forcing officials to repaint the graphics used to illustrate the bleak outlook for what is to come.
In October, fewer than 150 coronavirus patients were admitted to hospitals every day.
By late November, that number had doubled to about 300 patients a day – higher than in the entire epidemic.
And now it has doubled again, reaching nearly 700 new hospital patients every day, a few days before Christmas. This rate brings crisis to Los Angeles County.
If the behavior of disease transmission remains unchanged, the County Health Services Department’s projection says Los Angeles County could see between 700 and 1,400 new hospitalized patients per day by New Year’s Eve.
Daily hospital admissions for COVID-19 could rise tenfold compared to October
Roger Lewis, director of the COVID-19 hospital requesting a model for the Los Angeles County Health Services Department and a professor in the Los Angeles County Department of Health Services, said: “The model indicates that we could easily see 10 or more daily admissions than we saw in October. Emergency Medicine at Harbor-UCLA Medical Center in West Carson.
The Los Angeles County Health Services Department expects daily new hospitalizations for COVID-19 starting Wednesday.
(Los Angeles County Department of Health Services)
Indeed, the number of people infected with COVID-19 in Los Angeles County hospitals had nearly 5,900 as of Sunday – more than twice the peak summer during the second wave of the pandemic, as there were no more than 2,232 people hospitalized with the disease. Any given day.
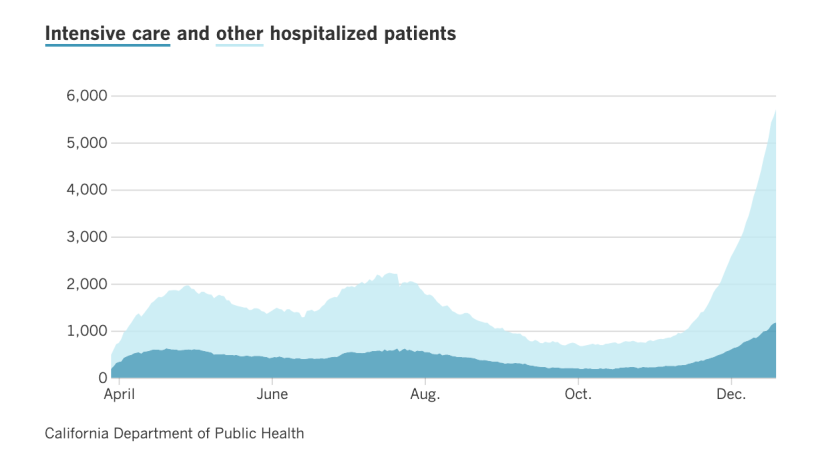
The graph shows the number of people hospitalized each day with COVID-19 in Los Angeles County.
(Los Angeles Times)
This means that by the end of the year, we could see up to 9,000 people with COVID-19 consuming Los Angeles County Hospital beds.
By mid-January, there could be 14,000 if there was no change in the transmission behavior.

Demand forecast for Los Angeles County Hospital Bed starting Wednesday.
(Los Angeles County Department of Health Services)
Of particular concern is the graph that displays the forecast of ICU requirements.
“We don’t have intensive care beds.”
Last week, the intensive care unit bed capacity available for COVID-19 patients in LA County ran out – the first time this pandemic has occurred.
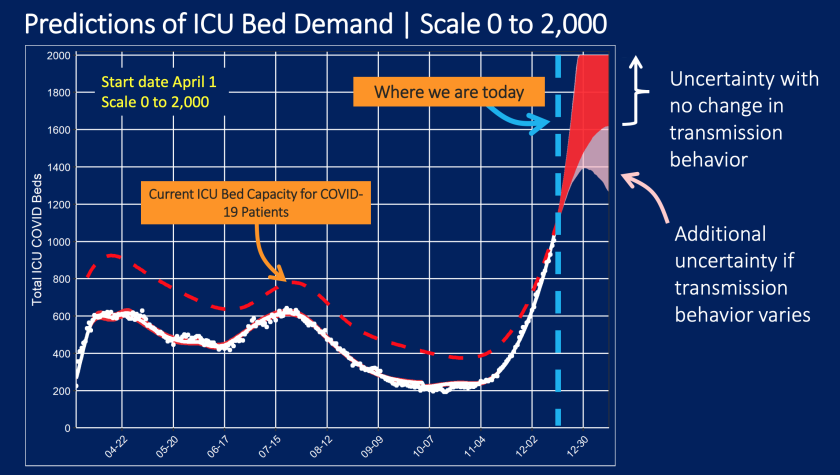
The ICU bed capacity available for COVID-19 patients actually fell to zero last week.
(Los Angeles County Department of Health Services)
“We are not providing ICU beds for additional patients at this time,” Lewis said.
More than 1,200 patients with COVID-19 in Los Angeles County were in the intensive care unit on Sunday, more than three times the number since late November.
Now, that doesn’t mean hospitals are not continuing to do everything they can to increase capacity. “There are limits to what can be done,” Lewis said Friday. “I think the biggest challenge facing hospitals in the next week or two will be the staff needed to care for patients with disease. COVID-19, who need higher levels of care. “
Los Angeles County is on track to record 110 COVID-19 deaths per day within weeks, public health director Barbara Ferrer said on Monday. The average number of deaths in the province currently stands at 84 deaths per day.
So what do hospitals do when there are no more beds available in the ICU?
Plenty of options for dealing with an ICU shortage – nothing is perfect
Among the options for finding ways to treat critically ill patients when the ICU is full:
- Requiring nurses to care for ICU patients more than usual. Usually, an ICU nurse takes care of one or two patients simultaneously. Nurses may be asked to care for three or four at the same time.
- Placing critically ill patients in physical locations outside the intensive care unit, such as keeping them in the emergency room for a longer period. “It’s not ideal to be in a physical location built to provide this level of care,” Lewis said.
“Having the system must accommodate this increased demand and do our best with what we have will not lead to good patient outcomes as we can achieve if we have less demand for care,” Lewis said. “Everyone does things differently than we would like to do ideally because there are more patients than we can take care of.”
This means that patients are at risk of worse outcomes. “This includes longer hospital stays, more time on a ventilator, and ultimately deaths,” Lewis said.
When there are too many patients on available medical staff, said Dr. Robert Kim Farley, an epidemiologist and infectious disease expert at UCLA Fielding School of Public Health, “there will not be the same quality of monitoring.”
Other temporary measures are not ideal. Kim Farley said that keeping patients in critical condition who need to be in the ICU waiting for the emergency room not only worsens the quality of care, but also creates a ripple effect that causes patients to wait in ambulances for hours outside the hospital. This leaves fewer ambulances available to take calls.
Fears of burnout
Fatigue is another major point of concern. The nurses are the ones sitting next to the ICU patients’ bed, and they are now being asked to work in higher intensity care settings than usual, to take care of more patients, ”and they would be required to do so for weeks on end, Lewis said.
So far, newly diagnosed coronavirus cases continue to soar in Los Angeles County and statewide, reaching or near daily record levels. This means that the frequency of infections that occurred during the Thanksgiving holiday and in people who were injured in these people is still on the rise.
Ultimately, a fraction of people who test positive this week will need hospital care – the state estimates about 12% of those who test positive statewide and 10% in Los Angeles County – and the average length of hospital stay is six days before recovering or the death.
“So the system will be required to care for more patients than it is today for at least the next two weeks,” Lewis said.
Two to three weeks to notice a change in behavior
“If everyone starts to be extraordinarily cautious today and the transmission is significantly reduced, the benefits of that – which will be enormous – will start to appear three weeks from now,” Lewis said Friday. “So, during the remainder of December, we expect to see … higher hospitalization counts and increased challenges for the healthcare system to provide the best possible care for most people.”
It can generally take about two to three weeks from the time someone is exposed to the virus until so sick that they need to be hospitalized.
“What is in our control is what happens in January,” Lewis said. If we do the right things now, January might be “no worse” than December. But if we continue to see the transmission the way it has been for the last month or so, January will be worse. “
When might we see evidence that the stay-at-home order has worked?
The big question is whether or not the territorial stay order that went into effect for most California residents on December 7 works.
Dr. George Rutherford, an epidemiologist and infectious disease expert at the University of California, San Francisco, said that when the COVID-19 lockdown orders went into effect in France, the United Kingdom, and Spain, “it took two to three weeks for the effects of the lockdown to even kick in.”
So this week, Rutherford will start looking at daily case rates to see if cases are starting to stabilize or perhaps declining.
Ferrer said she will start looking at trends around Christmas to see if daily cases are starting to decline.
Lewis said it will take until close to New Year’s Day for the stay-at-home order to start showing up in hospitals.
Kim Farley said it would be essential for people to say no to social gatherings during the winter break. “Are you invited to a party? Just say no. Are you invited to your friends to have dinner at their house? Just say no. That way, when you need an ICU bed, the hospital won’t tell you,” No.
The writer for The Times Mora Dolan contributed to this report.




:quality(85)/cloudfront-us-east-1.images.arcpublishing.com/infobae/ITUZQQXWI5ESDM7HV7TXONMIYM.png)
